What to Expect in Perimenopause and Menopause
If you’re a woman in midlife, you certainly know that menopause is coming, a natural biological process. It is diagnosed when your body has not had a period for one full year due to a drop in the main sex hormones — estrogen and progesterone.
The average age of menopause is 51, but it’s not uncommon to be in full menopause in your early 40s.
One million women experience menopause each year in the United States. Sadly, in a recent study, only about 6% of women feel prepared and many are less familiar with the term perimenopause, the 7 to 10 years leading up to menopause. This is the transitional time around menopause that can bring about a lot of changes, both physically and mentally.
Knowing what to expect and how to incorporate lifestyle choices to look and feel your best is the top way to tackle this stage of your life.

What to Expect in Perimenopause
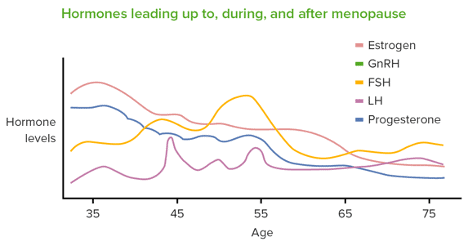
The start of perimenopause, in your 30s, 40s, or 50s, is when estrogen starts to decline. This then throws off the balance with progesterone. Both of these hormones are responsible for ovulation and menstruation.
Estrogen is not only important to your reproductive system but your body has estrogen receptors throughout the whole body. This means that a drop in estrogen causes symptoms that will be felt in many areas of your body.
No two women are alike, but it’s common for many women to notice many of these symptoms as hormones fluctuate in perimenopause and ultimately decline in menopause:
- Changes in periods (heavier or lighter and change in frequency)
- Night sweats / hot flashes
- Vaginal dryness
- Hair loss
- Joint pain
- Weight gain and a change in weight distribution
- Sleep disturbances
- Dry Skin
- Trouble concentrating
- Changes in sexual desire or painful sex
- Urinary frequency
- Headaches
It’s also worth mentioning that along with the above symptoms, low levels of estrogen and progesterone raise your risk for more serious health problems. These include heart disease, stroke, osteoporosis, urinary incontinence, and diabetes.
You must talk to your doctor about symptoms, health risks, tests for preventive healthcare, and lifestyle choices.

How Do I Know If I Am in Perimenopause?
If you are a woman in your 30s or 40s with many of the above symptoms, make an appointment with your physician to discuss the likelihood of being in perimenopause.
No one test or symptom will determine if you have entered perimenopause. Because hormones fluctuate greatly, it’s not always easy to get an accurate perimenopause diagnosis from bloodwork.
Since estrogen levels decrease in perimenopause, a woman’s follicle-stimulating hormone (FSH) naturally increases. Your doctor can check this level to help with a diagnosis. Be sure to bring a list of questions since it’s easy to forget once you are there.
Make sure your doctor performs tests to rule out other abnormalities that may cause some of the above symptoms:
- Thyroid examination and testing
- Pregnancy test (hCG)
- Blood work to check for nutritional deficiencies
- Prolactin test
- Iron deficiency
Lifestyle Changes to Help Improve Symptoms
Since the symptoms of perimenopause will interfere with your daily activities, it’s important to make changes to feel better. To help relieve symptoms and improve your quality of life during this time of hormonal changes, it’s necessary to make lifestyle changes:
- Eat well. Consuming a nutritious diet rich in vegetables, fruits, lean protein, healthy carbohydrates, and good fats will help balance your blood sugar and achieve a healthy weight. (I recommend intuitive eating to feel your best and maintain a healthy weight.)
- Get active. Exercise helps with bone, brain, and heart health. It boosts the feel-good hormone, serotonin, which will help you continue to make healthy choices!
- Quit smoking. Smoking contributes to heart disease and unhealthy skin and can damage your bones.
- Limit alcohol. Overconsumption of alcohol can prevent you from making healthy choices, and contribute to hot flashes and insomnia. Some studies have found a link between alcohol consumption and breast cancer.
- Get outdoors. Getting enough sunlight, especially in the morning, will also help with boosting serotonin, improving your mood.
- Dietary supplements. Many women can be deficient in nutrients as they age. Talk to your doctor about dietary supplements and doses that are safe to take.
- Manage stress. Elevated cortisol (stress hormone) levels or a dysregulated nervous system will worsen perimenopausal symptoms. Check in regularly on how you are feeling and when you are feeling overwhelmed. Ask for what you need, set boundaries, and say no when necessary.
- Embrace a mindful practice. Incorporate meditation, deep breathing, journaling, or yoga into your day to stay grounded and tap into your needs.
Do you want to do more than just survive in midlife?
Learn more about how to avoid the crisis and thrive in midlife in this insightful article on Middlescence.

Hormone Therapy for Relief of Perimenopausal and Menopausal Symptoms
Hormone replacement therapy (HRT) can help relieve many perimenopause symptoms, such as brain fog, hot flashes, joint pains, vaginal dryness, libido, and mood swings. This option should also be a part of the conversation with your doctor. Many women can begin this treatment if they are an ideal candidate as soon as it is confirmed that they are in perimenopause.
Basic types of HRT:
- Transdermal Estradiol patches, cream, gel, emulsion, injection or spray
- Estrogen vaginal cream or ring
- Oral Estrogen
- Micronized Progesterone pills
- Testosterone is beneficial for some women
The best practice is to take the lowest effective dose for the shortest length of time to relieve symptoms that are most troublesome.

The Menopause and Postmenopausal Journey
Menopause is the time that marks the end of a woman’s menstrual cycle. It is essentially one day. Most women will reach this stage in their late 40s or early 50s. Postmenopause is the stage you will be in for the rest of your life. You will no longer have a period, and hormone levels will remain low.
It’s important to note that menopause can either be naturally occurring or surgically induced, such as with a hysterectomy. A surgical procedure to remove the uterus. Both create symptoms due to decreasing hormones.
Seeing menopause as the beginning of the next amazing chapter can help make this a more positive experience. It’s a time when you need to tap into your symptoms, prioritize your health, and ask for what you need with increased wisdom. The more you understand your hormones, the better you will be able to manage your quality of life.
A time to truly thrive and not just survive!
I would love to hear your perimenopause or menopause story. Please share your challenges and what things you put in place to improve your symptoms with us in the comments below. I am happy to answer questions as well and support you in your journey through midlife!

Featured Author
Kathleen of Women and Balance
Hi, I’m Kathleen McDermott. I’m a nurse with a master’s degree in nursing education and a certified women’s health coach who helps women manage menopause symptoms and make peace with food by eating intuitively! I also freelance as a writer and speak to women at local businesses to help them understand their changing hormones and truly thrive in midlife! You can find me at womenandbalance.com, Instagram and LinkedIn.




